When it comes to employee benefits, does your organization clearly lay out what your workforce has access to when it comes to their health and well-being? A recent study suggests that access to benefits can often be intimidating for employees, impeding utilization and plan participation rates. Deterrents include a poor understanding of what benefits are available, how to access them, and insufficient coverage where it matters most.
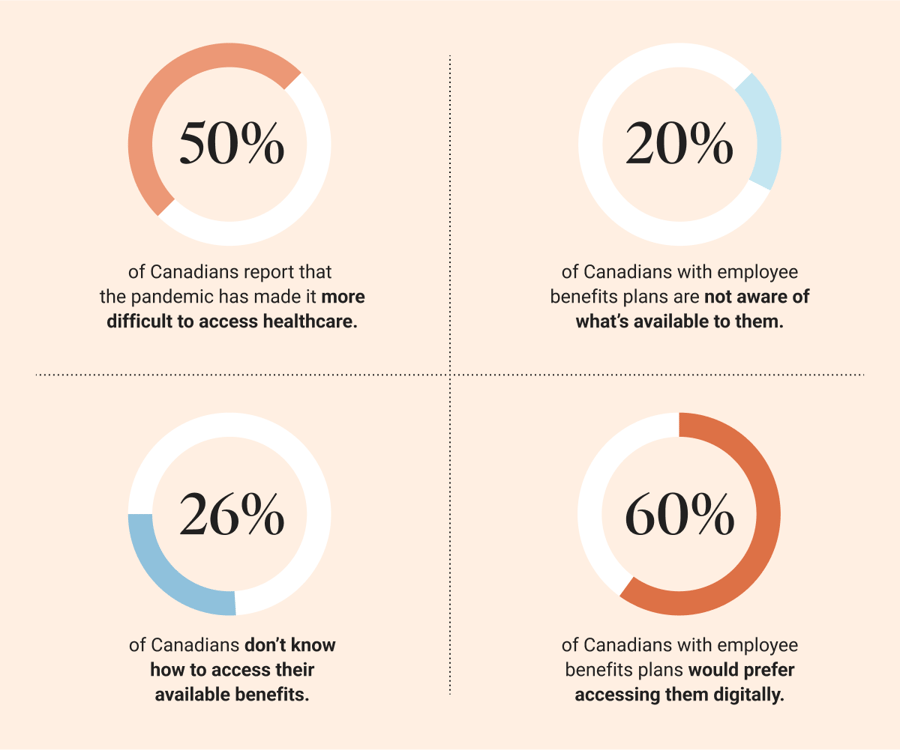
Between an increasing number of barriers to care and not leveraging the help that’s available to them, employee wellness is left hanging precariously in the balance. Organizations must promote awareness around employee benefits and reevaluate their providers because:
Poor plan participation rates waste precious corporate funds and can seriously affect employee well-being if they aren’t finding the help they need. Dialogue’s virtual care solutions ensure members have direct access to benefits through industry-leading technology, delivering care through our multidisciplinary team of practitioners, and implementing employee engagement plans. How can organizations increase benefits utilization among employees to drive positive health outcomes in the workplace?
Painting the plan participation picture
Almost a third of Canadians with employee benefits plans indicated not having, or not being aware of, an employee assistance program (EAP). And among those who do have access to one, almost 60% have never actually used it. Employees might lose steam searching for inclusions hidden in the end pages of benefits handbooks. They can’t be blamed, either: these pay-per-use models don’t encourage employers to promote costly benefits. Finding out what’s actually available becomes challenging, putting utilization in the employee’s court.
Conversely, per-employee-per-month (PEPM) models like Dialogue’s encourage employees to leverage the benefits in their plans without paying out-of-pocket, in line with 86% of Canadians’ expectations. What’s more, our services are available until members reach remission (while our primary care program is unlimited), incentivizing employers to justify their investment by driving utilization and promoting workplace wellness.
How removing barriers to care improves plan utilization
The next frontier of virtual care is the use of data and technology to track positive health outcomes, and to build better models to reduce barriers to care for your employees.
Technology’s leading role in utilization rates
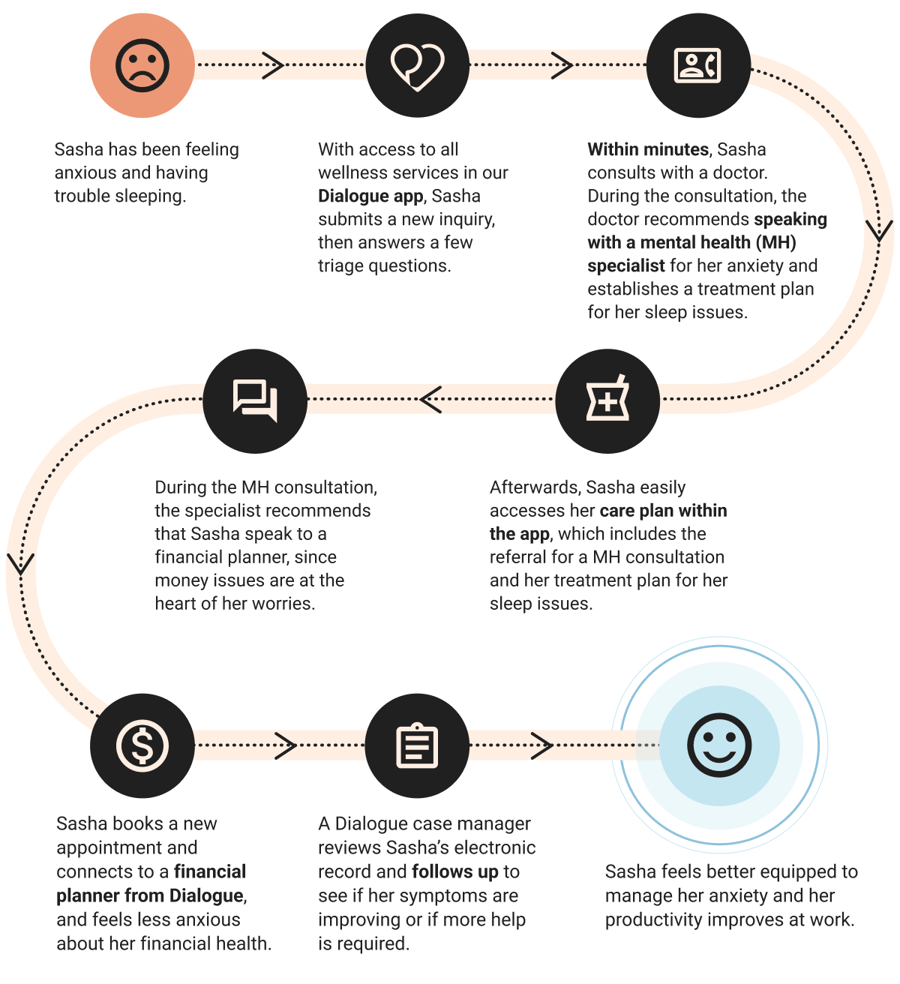
Accessing employee benefits can be made challenging by technological barriers: plans are difficult to access and outdated (like offering in-person consultations, or only being available via a 1-800 number), diluting the likelihood of a timely resolution for issues. Choosing the right technology is crucial to delivering quality care. We provide consultations through secure video, and follow-ups for results or appointment confirmations are done via Dialogue’s chat functionality or by phone.
Through the use of our app, 100% of symptomatic members requiring a follow-up get one to determine if they got better, stayed the same, or got worse. Those who haven’t improved will receive a follow-up with a medical professional; we close the loop on all issues, including those requiring members to be seen in person. This also means that for chronic or longer-duration issues like anxiety or depression, a member will feel supported and be more likely to complete a treatment program, either preventing or reducing disability duration and increasing recovery rates.
Generate positive member experiences
Virtual care promises to deliver the right care to the right member at the right time and according to the member’s treatment preference. 66% of Canadians agree that the future of healthcare is virtual, preferring to meet virtually over attending in-person consultations.
Dialogue’s triage system determines the suitability of virtual treatment, prioritizing patient safety and preventing the doubling of care (such as determining, after a virtual consultation, that an in-person evaluation is necessary after all). Dialogue can safely treat over 70% of non-urgent medical issues with real-time access to our multidisciplinary care team. And when it comes to mental health treatment preferences, 73% of Canadians want to access self-led resources instead of attending a face-to-face session with a mental health practitioner. There are no differences in health outcomes between attending virtual or in-person therapy.
In today’s competitive labour market, employee experience and satisfaction with their benefits are just as important as ROI. Improving access to benefits and creating positive interactions:
-
Empowers employees to get help when they need it, providing follow-ups to track progress and offer additional support;
-
Reduces the cost associated with presenteeism (showing up for work when unwell) and absenteeism (spending hours away from the office to attend appointments);
-
Promotes an environment that values employee well-being;
-
Attracts new talent and preserves retention; and
-
Improves the perception that the employer prioritizes employee well-being.
Reduce wait times to receiving care
Dialogue’s user-friendly app, combined with the expertise of Canada’s largest multidisciplinary care team available 24/7, means our members can receive care within minutes. At a time when almost 50% of Canadians report having to wait 4 days or more to see a healthcare professional for minor health issues, access to timely care and flexible scheduling is a major advantage. Our administrative process is 5x faster than that of the traditional healthcare system.
When it comes to mental health, the onus often falls on the employees to research and find a specialist, facing long wait times exacerbated by the pandemic. 39% of Canadians seeking mental health help waited 8 days or more to see a mental health specialist, yet 52% of Canadians wish they’d receive help the same day they need it.
Dialogue reduces wait times to as little as 24 hours, and members can select the most convenient date and time. Timely, preventative mental healthcare through Dialogue allows organizations to experience a 5x ROI by avoiding disability leave. Our solutions reduce short-term disability to less than 6 weeks in 70% of cases (compared to a Canadian average of only 30%).
Providing holistic care that adequately responds to member needs
Well-being doesn’t stop at physical and mental health. Health concerns and life events are often intertwined. Holistic care makes sure members have access to services that correspond to multiple definitions of wellness.
Dialogue’s IHP: manage benefits in one place
Organizations can fill the gaps in employees’ understanding of their benefits plans by consolidating all services into one app. Dialogue’s Integrated Health PlatformTM (IHP) provides single login access to all programs, promoting awareness and reducing delays in receiving care. Our unique platform is proven to provide positive health and business outcomes, with an average of 4.2 hours of absenteeism saved for each episode of care. More importantly, employees are 77% more likely to seek help using Dialogue’s integrated app.
Our collaborative care model provides support for physical, mental, financial, and legal wellness, casting a consistently wider net of treatable issues. Easy access to ancillary services leads to a timely assessment of complex encounters and positive results, improving member outcomes, decreasing corporate costs, and reducing barriers to care.
A dedicated multidisciplinary care team focused on longitudinal, member-centred care
Longitudinal care manages high-risk, complex cases over an extended period of time. When a member consults with Dialogue, an entire team is behind the practitioner, increasing the likelihood of finding an expert on any topic. Our practitioners consult each other to add value to a case or consider additional insights.
This is only possible because Dialogue’s care team is an integrated, vetted and trained part of our workforce. In contrast, other virtual care providers use an external network of practitioners who may not be able to communicate with one another for quick peer-sourced input.
Encouraging your employees to use their benefits
Dialogue’s virtual care solution includes a tailor-made onboarding plan by our customer success team, ensuring employee engagement is set up for success. We offer in-depth reporting and insights into program participation, helping HR leaders and organizations determine if the platform is being used optimally, or identify new communication opportunities.
Proactive onboarding
A dedicated Dialogue onboarding specialist will accompany your organization from pre-launch, to go-live, to post-launch, and equip you with all the tools and content you’ll need to successfully promote our programs.
Our team tailors communication plans to your organizational needs and the overall preferred communication channels of the business. We customize the launch according to your organization’s reality: for example, if emails may not be well received by employees, we offer alternative ways to connect and curate that content to fit the reality of your environment.
Employee engagement planning
Dialogue’s account managers know that not all employees necessarily need their benefits right away. We identify key moments in your organizational calendar where it may make sense to promote Dialogue and tie it back to real-life events (like flu season, back-to-school, or Mental Health Week).
Internal buy-in is the most effective way to boost plan engagement. We pay particular attention to who you would identify as your organization's internal ambassadors, since they would be best positioned to promote the plan among your employees. Should spreading the word about Dialogue come from the managers, C-suite, or the Heath & Wellness Committee members? We then deliver custom messaging based on what's worked in the past and your current reality, and make recommendations for the best ways of promoting and using Dialogue.
We’ll also equip you with an onboarding and engagement toolkit, which includes:
-
Onboarding webinars
-
Marketing materials (emails, posters, computer background images, introductory videos)
-
Communication materials for internal distribution
-
Onboarding and monthly engagement emails about Dialogue and special health and wellness campaigns
-
In-app resources
Wellness reporting and metrics to track program success
Our programs offer integrated wellness reporting (data availability dependent on client size to protect confidentiality) which can be used for a multitude of reasons.
-
Our clients at Digital Extremes share our reports with their leadership team to provide insights into utilization, satisfaction and ROI.
-
PSP uses Dialogue’s tracking to keep an eye on employee well-being, with an 11x ROI on our mental health program alone.
-
At Via Rail, a team of internal ambassadors regularly communicates news or updates about Dialogue to employees, saving 3.8 hours away from work per employee per care episode.
Aggregated reporting allows easy monitoring of progress and provides insights into areas of improvement. You’ll monitor program performance, like member adoption and utilization rates, and work with your customer success account manager to implement strategies to continue generating positive results. These metrics are compelling indicators to share with your organizational leaders to illustrate return on investment.
Improving employee benefits plans participation rates is a win-win
Improving participation rates in benefits plans means employees get the help they need when they need it, and organizations benefit from the resulting renewed productivity. For HR professionals looking to promote corporate wellness, build healthy, productive teams, and offer competitive benefits packages, Dialogue can:
-
Decrease the time spent waiting to see a healthcare provider to 24 hours, reducing time spent away from the office as a result
-
Avoid confusion by centralizing all benefits in one single login platform to boost utilization rates and provide quick access to support
-
Reduce absenteeism and improved employee performance by saving an average of 4.2 hours of absenteeism for each care episode with Dialogue
82% of working Canadians expect their employers to offer virtual care, and responding to that request might improve utilization rates, too, with 60% of Canadians claiming they would actually use their plan if it were offered virtually. Is your organization ready to rise to the challenge? Make employee wellness a priority today.
Ready to discuss how Dialogue can help your organization achieve positive health outcomes and a stronger bottom line?




 Canada (EN)
Canada (EN)
 Global (EN)
Global (EN)








