-
Integrated Health Platform
Overview
-
Integrated Health Platform
Improve the overall health and wellness of your organization with a single, modern platform.
-
How we're different
We drive real member outcomes through virtual care and Humanized Healthcare.
-
Our clients
Improve productivity, reduce absenteeism, and build a culture of happiness and well-being.
Programs
-
 Employee Assistance Program
Employee Assistance Program
Essential wellness services to stay happy and healthy, in one digital-first platform.
-
 Mental Health+
Mental Health+
Flexible, integrated, and personalized mental health care, backed by science.
-
 Primary Care
Primary Care
A complete member journey accessible from our industry-leading virtual care platform.
-
 Wellness
Wellness
Empower all of your members to proactively adopt healthy habits.
Features
-
Women's and Family Health
Coming in 2026: Be among the first to explore Dialogue’s newest care offering.
-
EAP cost savings calculator
Measure what matters with Dialogue's EAP Cost Saving Calculator
-
 Health and Well-Being Report
Health and Well-Being Report
Discover the key lifestyle factors affecting your members’ health and learn how to strengthen your organization’s well-being.
-
-
Why Dialogue
Dialogue Experience
-
For organizational leaders
Discover how we can help drive positive outcomes for your organization.
-
For partners
Elevating Canadians’ healthcare expectations, together.
-
For members
Members can expect a better experience compared to traditional employee benefits and care.
-
 Healthiest Workplace Awards
Healthiest Workplace Awards
Recognizing Canada’s top organizations leading the way in employee health and well-being.
Why Dialogue
-
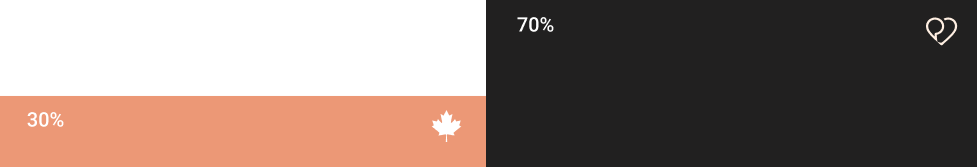
 Discover your savings
Discover your savings
High-quality, virtual benefits for your employees aren’t an expense - but an investment
-
Why virtual care?
Explore the positive impact of Dialogue's virtual care.
-
Ultimate Guide to EAP
Learn how Dialogue is reinventing the EAP experience.
-
About us
Dialogue is the leading health and wellness provider in Canada.
-
-
Resources
Learn
-
Resources centre
Discover the latest news, content and reports for HR leaders.
-
Blog
Learn more about health, organizational well-being, and life at Dialogue!
-
Case studies
Learn how we improve the health and wellness of our clients.
-
 Newsletter
Newsletter
Stay a step ahead on employee benefits, wellness, and productivity news and resources.
Support
Overview
The cost of neglecting women’s health
Watch the recordingWe’re spotlighting women’s health stories and unveiling something big.
2025 State of workplace well-being
Download the reportData-driven insights on employee well-being, and how you can make informed decisions for your organization’s EAP.
-
-
Get Pricing



 Canada (EN)
Canada (EN)
 Global (EN)
Global (EN)



































.png)

.png)

%201-1.jpg)
%202.jpg)


.jpg)



.jpg)


%204.jpg)
%205.jpg)



-1.png)

%206.jpg)
%206%20(2).jpg)
%206%20(1).jpg)


-1.png)



.png)


